Intra-muscular shots are relatively easy to give to your horse due to the horse’s huge muscle mass. This makes it easy to hit the muscle and harder to hit other vital structures such as the spinal cord, bone, or blood vessels. Before trying to give a shot in the muscle, it is important to keep in mind a few key facts.
LOCATION, LOCATION, LOCATION You can either give the shot in the neck or in the rump, or both, depending on the demeanor of your horse and your preference.
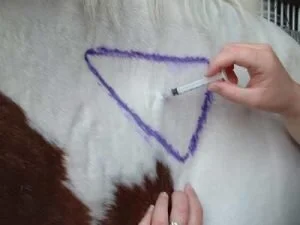
There is a triangular shaped area that is used for IM injections in the neck. If you imagine a line a hand’s breadth below the crest of the neck, a hand’s breadth in front of the shoulder, and a hand’s breadth above the groove where the jugular vein runs, this will form a triangle. You can inject anywhere in this area.
Stay a hand’s breadth below the point of the rump, and above a line level with the stifle. You can inject anywhere in this region, as long as you do not go right in the crease between two muscles. Stand right next to your horse when you do this, with your hip right against his side. It is always safer to have someone holding the lead.
GIVING YOUR HORSE A SHOT - STEP BY STEP
Step 1.
Always take the needle off the syringe when you go to stick it in your horse. This will allow you to readily see if you inadvertently hit a blood vessel, and will also prevent breaking off the needle or wasting some of the medication.
Step 2.
Be bold when you stick the needle in! The horse’s skin is almost ¾” thick, and the more timid you are, the more times you’ll have to poke your horse just to get it through his sensitive skin. Take a pinch of skin above the injection site to distract your horse from feeling the needle. Make sure you push the needle all the way into the hub. Otherwise, as you are injecting you may accidentally push it further in and hit a blood vessel
Step 3.
After sticking the needle in, attach the syringe and pull back on the plunger to make sure that there is no blood.
Step 4.
Push the plunger forward to inject the medication into the muscle.
When you give your horse a series of shots, such as a course of antibiotics, rotate side to side when you give the shot in order to prevent sore spots. If you always think “right (side) at night”, no matter whether you give the shot in the neck or rump, you will avoid giving it in the same spot in the morning and at night.
Original Content - https://gvequine.com/how-to-give-intra-muscular-injections/